Regardless of our race, religion, gender or age, we all have something in common: We’re all going to die.
My friend Eve Elting passed away eight months ago, after she stopped treatment for metastatic breast cancer. At 58, she’d had cancer for 20 years. “I’ve been on 13 different chemotherapy agents,” she told me. “Enough is enough.”
Eve’s decision to die started me thinking about how people view their mortality. What makes us fear death? Why are some people not afraid? What can help us face this natural part of life with more ease?
As an oral historian, I often interview people in the last chapter of their life, either because of age or a terminal illness. I hear stories of their life and experiences, including the impact of family members dying and their own attitude about mortality.
“When I was young I was terrified of dying,” Gladys Sturman, 85, said. “My mother got cancer when she was 50. We were all sitting there crying, and she says, ‘Why are you crying? Kings die. Presidents die. What? Did you think I wasn’t going to die?’ When she said that, it totally lifted my fears.”
When Dave Schwartz was 100, he said, “There are times when I’m very brave, and I reconcile myself to my demise. I think, it’s a passage; all living things have a beginning and a biological end. I’m looking at things rationally. But there are other times when I have a sense of sadness, a sense of nostalgia, and I have to admit, a sense of fear.”
Discussing end-of-life wishes
Starting in her 70s, my mother, Marcia Goodfriend, was adamant about one thing: “Promise me you won’t let anyone keep me alive with a machine.” She repeated this in letters and on visits and sent my sister and me copies of her Living Will. We knew what Mom wanted before she died, which made our lives easier.
Far too often, these conversations don’t happen. Yes, it’s awkward and it involves admitting that someone is going to die, which is painful. But otherwise, family members are faced with impossible decisions to continue or stop their loved one’s treatment.
“It can be very liberating to have this conversation,” Rabbi Ed Feinstein of Valley Beth Shalom said. He learned he had cancer when he was 39 and, in his 2013 Yom Kippur sermon, he told his congregation, “You need to communicate with your loved ones what you want your final days to be like. What do you need for a reasonable quality of life? When should the fight for your life be carried forward, and what are you willing to endure? And when would it be permitted to say, ‘Enough?’ ”
Having difficult conversations
“Cancer is an illness of families, and the whole family is suffering terribly,” oncologist Daniel Lieber said. “I think people are afraid the patient won’t be able to handle hearing what their family is feeling and vice versa. But that is really isolating.”
Lieber’s father, Rabbi David Lieber, died in 2008 from a lung disease. “He faced his mortality with open eyes, which was incredible,” Lieber said. “Many people say, ‘Why me?’ and my father said, ‘Why not me?’ I could say to him, ‘I just can’t believe what it’s going to be like when you’re no longer alive.’ We knew that we could talk to each other that way.”
Renee Marcus’ husband, Richard Marcus, an account manager in the storage and networking computer industry, died from pancreatic cancer at 68. “We talked about everything,” she said, “and that continued during the nine months after his diagnosis. I thanked him for not dropping dead of a heart attack, so that we had time to talk. I have nothing left that I would have said to him. When I joined a bereavement group, people were envious of me, because they hadn’t talked like that. They thought they’d have the time to do it, but they procrastinated.”
Numerous resources exist to assist people in facing their fears.
Ronnie Kaye, a psychotherapist in West L.A. and herself a cancer survivor, sees many people dealing with mortality. “Each person carries a set of issues related to sickness and mortality,” she said. “No matter what age, I ask, ‘Tell me what scares you?’ It’s opening the dialogue, not knowing where it will lead, but convinced that anything they open up is something we will be able to manage together.”
It’s not unusual for someone facing the end of their life to express anger, Kaye said, and this is especially true with young adults or teenagers. “There is an extra ingredient, because it’s not the right time; there was so much more life to live. In contrast, I often hear from an old person, ‘I’ve had a good life.’ ”
Meditation, or “mindfulness,” is believed to help ease the emotional turmoil of facing illness or mortality. Arash Asher, director of Cancer Survivorship and Rehabilitation at Cedars-Sinai, agrees. “It really is about being self aware and differentiating what our thoughts and feelings are from reality, and having some sense balance in relation to that.” Finding such resources is one of the services offered by Dikla Benzeevi, a patient navigator in Studio City. “I guide them through the journey,” she said. “What’s the most critical thing to do now? What’s the best way to go about the next steps? What can you learn? Where can you get support? I talk about the best approach and help them find resources.”
Counseling both the dying and their family is something Feinstein does often. “Someone came to me when his father was dying. He expected me to have some sort of prayers or mystical rituals to carry out, and I said, ‘Yes, we have them, but it’s more important that you hold his hand and he hears your voice talking about your children and how he’s affected them.’ What we’re tying to do is to re-humanize death. By recognizing that death is what happens to us all, it gives people the courage to help each other through that.”
What might be needed in a family, Rabbi Elie Spitz of Congregation B’nai Israel in Tustin said, is encouragement to be honest about a loved one’s condition. “If I’m with a family that’s withholding that information, I counsel them to share it. The context of last words to someone who’s dying is acknowledging on both sides that the end is near. It’s essential for your relationship and closure that there is honesty and partnership.”
Doctoring
“Doctors are in the business of healing and tend to focus on that rather than acknowledging the end is near,” Spitz said. “That’s where palliative care doctors will say, ‘Here are your options and you might choose to die with less pain by not having heroic measures.’ ”
Lieber agrees. He presents treatment options – the pros and cons – and talks with patients about whether the treatment is worth it. “People are not looking for just the technical. They want to know that you care and will discuss the options and value judgments with them.”
Kaye recalled a special example of doctoring. “I was sitting with a patient in the hospital when Dr. Av Bluming came in. The patient said, ‘Am I dying?’ and he said, ‘Yes, you are. What questions do you have for me about that?’ The only thing she wanted to know was, ‘Will it hurt?’ and he said, ’It’s my job to see that it doesn’t.’”
A word about hospice, or end-of-life palliative care: My mother spent her last years in a board-and-care home. Twice in her last month, they rushed her to the hospital, which was not what she wanted. I discovered that getting Mom into hospice would allow her to stay in her room at the board and care, which was now her “home.” She died there, with my sister and me telling her we loved her and singing her favorite Broadway melodies.
Faith, God and Yom Kippur
For some, faith can help lessen the fear of dying, but if one believes a terminal illness is a punishment from God, it can be confusing.
“I don’t think God gives us cancer,” Feinstein said. “The disease is the human condition that we live with. To me, God comes into it when a doctor walks into my room at 5 a.m. to make sure I’m OK, and when we live lives of meaning and take care of each other. My faith, when I was diagnosed, focused on the people around me and reminded me of the many blessings in my life.”
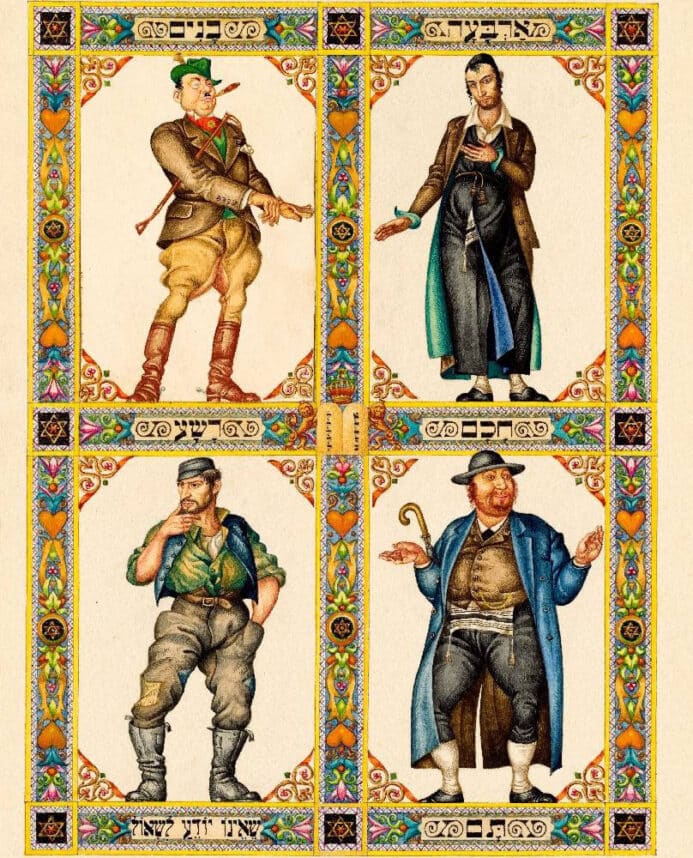
The traditional Yom Kippur liturgy suggests that if one is not forgiven by God, he or she might not live another year. This can be frightening for someone with a terminal illness.
“The liturgy comes from a different world,” Feinstein said. “Rabbis have always reinterpreted ancient sources for their contemporary times. I had wrestled with those prayers and, after my diagnosis, I found new meaning in them. I understood why they needed to be reinterpreted when a person is struggling with life and death. The holiday asks you, if you had only 25 hours to live, what would you want to accomplish? What would you want to say? That’s what Yom Kippur is about.”
Added Spitz, “The wisdom of our tradition is that Rosh Hashanah celebrates the creation of life, and Yom Kippur is the taste of death. The 10 days between the holidays offers a mini life cycle that gives us the perspective from both sides of life … the beginning and the end, leading us to know about the value of our lives.”
Finding meaning
Eve wanted to have a “good death.” She reminisced about her family, her challenges and successes, her friendships and life’s lessons. She expressed gratitude to people she loved, and she forgave both herself and others. She truly modeled finding and creating meaning before dying.
Asher started a program at Cedars-Sinai to increase people’s emotional wellbeing when facing cancer. “Even though one is in this serious situation,” Asher said, “there are still things that they can be grateful for. You can still define your own legacy and find meaning in things that are very important to you. You still have the capacity to love and to laugh.” Asher’s program is called Growing Resiliency and Courage with Cancer, or GRACE.
Benzeevi, the patient navigator, has noticed that a serious diagnosis can inspire positive life changes. “When people receive a metastatic cancer diagnosis, they may experience a major transformation. They let go of toxic relationships and create more nurturing ones. They alter their life style. Their perspective changes; things that used to aggravate them are not as important. Their priorities change. They live life at a more experiential level, with a deeper mindfulness of the moments in their day and week, and of their relationships.”
In February, the neurologist and author Oliver Sacks wrote in The New York Times about his terminal diagnosis. “It is up to me now to choose how to live out the months that remain to me. I have to live in the richest, deepest, most productive way I can.
“I have been a sentient being, a thinking animal, on this beautiful planet, and that in itself has been an enormous privilege and adventure.”
Ellie Kahn is an oral historian, award-winning documentary filmmaker and founder of Living Legacies Family Histories, www.livinglegaciesfamilyhistories.com, which produces audio and video of oral histories for families and organizations.



















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.