
The Biden administration’s announcement of ten high-cost Medicare drugs slated for price negotiations reminded me that the program’s part D drug benefit should be termed “Medicare F” for the way it fails seniors like my patient Bill.
The problem started with the program’s approval in 2003. Passed under President George W. Bush, its Republican authors complied with Pharma’s insistence on prohibiting Medicare from negotiating drug prices. Instead, the program delegated negotiations to numerous private Part D plans, none with sufficient economies of scale to bargain effectively.
Bill is an 85-year-old immigrant who has done well for himself and his family. He raised five children along with his wife, who passed away seven years ago. He thought he had sufficient retirement income to maintain a home and cover medical expenses. But then he developed an Ozempic problem. Taken along with the generic drug metformin, Ozempic controlled his diabetes. That was great except for Ozempic’s $10,500 annual price tag. Under his part D plan, Bill’s share was about $4600. That was a deal breaker for a retiree on six other prescription drugs.
Novo Nordisk, the drug’s producer, has an assistance program for low-income patients, but Bill failed to qualify, though he’s far from affluent. Prior to his most recent appointment, he stopped using the drug. His blood sugar control rapidly deteriorated. We then started an older drug from a different class but so far it hasn’t worked.
Prices negotiated by Medicare on this year’s drugs won’t go into effect until 2026.
As Ozempic ranks tenth for total Medicare drug expenditures, you might think that the Biden administration’s price negotiations would rescue Bill from his Ozempic problem. You’d be wrong. Under the process set out by the Inflation Reduction Act, only ten drugs that were approved at least seven years ago can become eligible for negotiation. Ozempic becomes eligible in 2024. Worse yet, prices negotiated by Medicare on this year’s drugs won’t go into effect until 2026.
The baby steps Medicare initiated to assist seniors in the future have long since been taken elsewhere. In France for example, the government routinely negotiates drug prices. Not surprisingly, French drug costs are less than half of what U.S. consumers pay. A study in 2017 showed that if Medicare paid French prices on just six drugs it would have saved $5.5 billion.
Pharma fails to appreciate the break it gets from the go-slow approach that negotiates prices after seven fat years, then allows two more before negotiated prices take hold. The drug companies have filed multiple lawsuits to block negotiations. Although I’m not a lawyer, their legal arguments make little sense. They argue that negotiations violate their rights under the Fifth Amendment, which prohibits the taking of private property without just compensation. Common sense dictates that Medicare, the purchaser, should help set the prices it pays. The fact that negotiation was delegated to private Part D plans would not make it unconstitutional for the program to assume that role itself. The process should be no different than the drug price negotiations the government currently conducts for its Veterans Administration system. Pharma’s legal arguments seem less about legal drug pricing and more about prolonged judicial processes that keep profits flowing.
Drug companies also claim that reduced profits might curtail future research needed to create novel drugs. Consider Bristol Myers’ Eliquis, a drug approved in 2012 that is now Medicare’s most expensive. It brings in about $9 billion annually. The company earns enough to pay its CEO, Giovanni Caforio, nearly $20 million annually. One might ask Caforio, whose fellow Pharma CEOs earn similar salaries, when is enough, enough? Negotiated prices won’t reduce profits to zero. And, if the companies want to mitigate the hit to their U.S. profits, they might negotiate better deals elsewhere so that Americans like my patient Bill no longer subsidize patients in Europe.
Doctors and patients understand and respect the value of the life sustaining drugs that Pharma produces. Still, that cannot justify Pharma practices that save lives with one hand while blocking access with the hand that grasps for every dollar of profit. We can only hope that the Biden administration will fight effectively for consumers and that the courts will speedily inform the drug companies that price negotiations are a standard business practice in the U.S. In the interests of the patients and the public, it’s time to bring Pharma to the table.
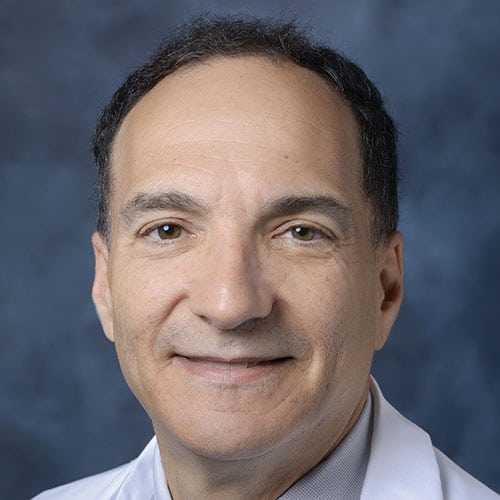
Daniel Stone is Regional Medical Director of Cedars-Sinai Valley Network and a practicing internist and geriatrician with Cedars Sinai Medical Group. The views expressed in this column do not necessarily reflect those of Cedars-Sinai.



























 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.