
My patients sometimes comment on the notion that doctors’ education neglects the study of nutrition. But while they are quick to point out this gap, they seldom mention an issue that is given far less attention: fashion!
Despite growing up with a mother and two sisters who often dressed to make a statement, it’s hard to imagine anyone less fashion-oriented than me. My distant memories include dreaded shopping expeditions with my mother who would select an absurd item of clothing and proclaim it “just what they’re wearing.” My retort, probably as soon as I could speak, was, “who are ‘they’ and why should I care?” Then and now, my usual fashion statement could be issued by a political spokesperson: “no statement at this time.”
Despite my fashion allergy, patients occasionally comment favorably on my apparel, typically a tie that complements a shirt. I usually respond by inquiring about whether their ophthalmology care is up to date. When truly cornered, I’ll pipe up with something like, “Sometimes one hits the ball even while swinging with the eyes closed.“
Given this attitude, recently I was surprised to discover myself opining publicly on doctors and fashion. My medical group had asked those of us with three decades of tenure to offer lessons gleaned from thousands of hours of patient care. Charitably, they allocated twenty minutes.
Not surprisingly, there has been research that shows that patients prefer doctors to dress somewhat formally and wear a white coat. But the pandemic, whose influence seeps into every corner, altered that dynamic. Doctors doing video visits could now dress however they pleased, at least from the waist down. I’ve taken advantage of this, too, and on video visit days, I’ll wear jeans with a long-sleeved shirt and tie. As informality spreads like a virus, we now see doctors in the office either dressing like they would at home or wearing surgical scrubs.
How difficult is it, I asked my colleagues, to take the few extra minutes to reassure those who might care? That’s not fashion, it’s compassion.
I would concede to my less formal colleagues that down-home attire would not offend long-term patients whose confidence is long established. But new patients make judgments based on the first visit. For male physicians, wearing a tie reflects an understanding that patients feel more at ease with someone who looks “on their game.” Particularly for seniors, that traditionally translates into wearing a tie. How difficult is it, I asked my colleagues, to take the few extra minutes to reassure those who might care? That’s not fashion, it’s compassion.
Of course, women are off the hook on the tie issue. But professional attire still matters for anyone in healthcare.
Scrubs? There are three reasons to wear them. In the operating room, ordinary clothing generates airborne contaminants, so scrubs are required. In an emergency department, clothes may get stained from procedures. But neither issue applies to outpatient primary care. I suspect that patients realize that primary care doctors wear scrubs because it’s more comfortable to work in pajamas. Although they make dressing easier, scrubs also contribute an aura of urgency and time constraints appropriate for an emergency department. Outpatient care should be more about deliberation. We may not need a pipe and tweed coat, but a long sleeve shirt and tie, or the female equivalent, makes sense.
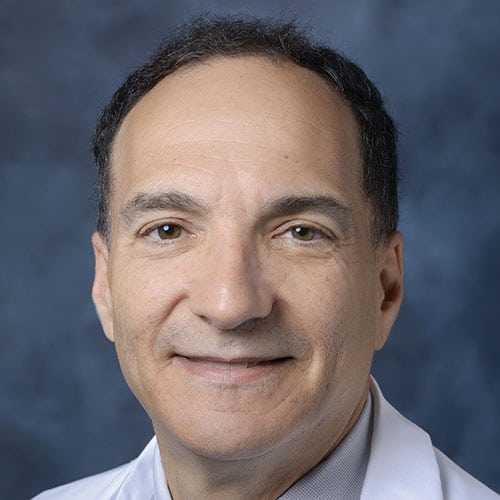
As a confession, I wear a white coat only for photo ops or special circumstances. The Almighty set my thermostat a bit high and with the extra layer I rapidly over-heat. I recently assisted in a clinic administering Evusheld, an injectable medication that protects immune-suppressed patients from COVID. As the patients didn’t know me and with the benefit of some extra “cooling time” I donned a white coat even though it felt like a Marcus Welby Halloween costume.
A week after the talk for my colleagues I observed no discernible difference in their dress habits. They would probably change ingrained personal habits only for mortality risk or a threat to compensation. And probably not in that order. But that’s OK. After over three decades, I’m used to people not taking my advice. It’s an occupational hazard, both the patients’ and mine. I’ll continue to plod along as a slightly formal medical dinosaur and plan to hang up my stethoscope, tie and bullhorn at the same time.
Daniel Stone is Regional Medical Director of Cedars-Sinai Valley Network and a practicing internist and geriatrician with Cedars Sinai Medical Group. The views expressed in this column do not necessarily reflect those of Cedars-Sinai.




















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.