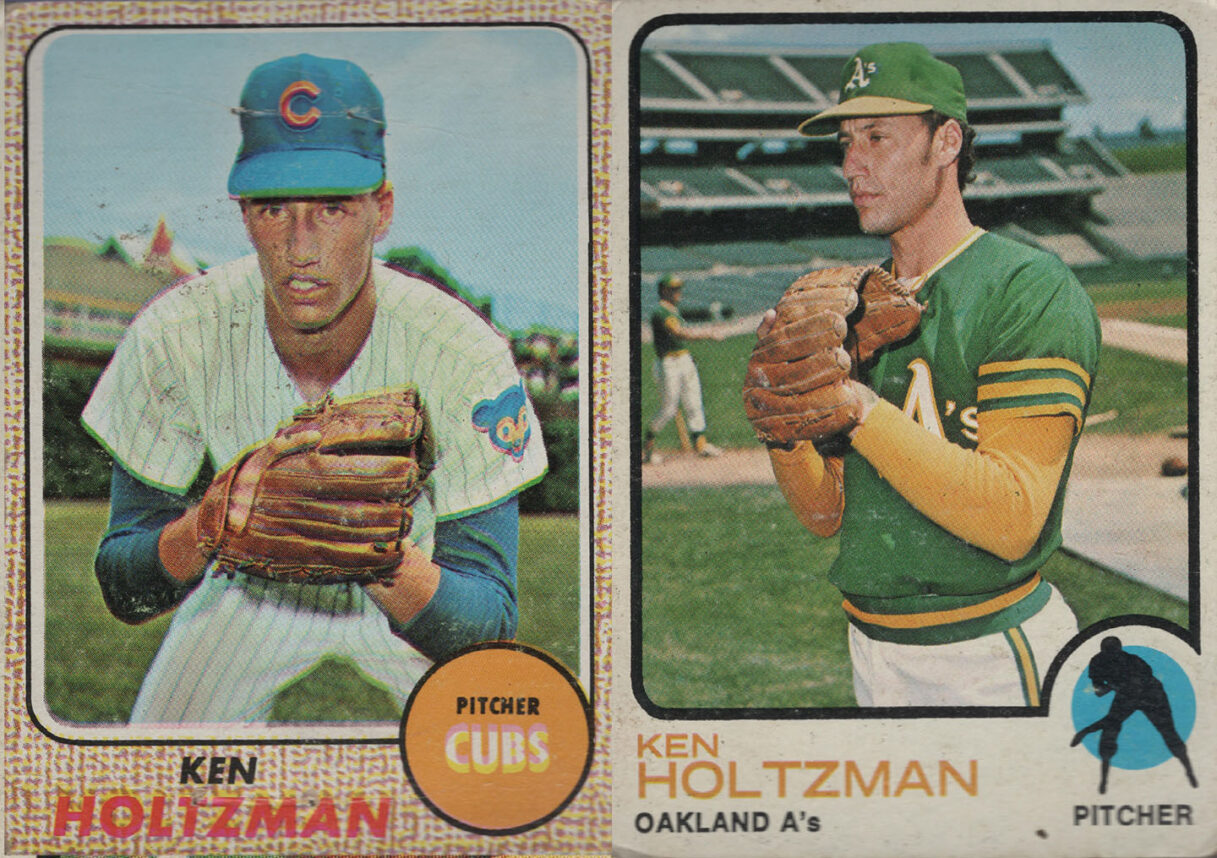
Sally H., an 80-year-old Fairfax resident, recently fell into inconsolable sadness after her canary died. To her family, her intense and prolonged sorrow seemed out of place because Sally had only bought the pet a few months earlier.
“It was only a bird!” they said.
What her family didn’t realize was that the loss of her canary reawakened decades of unfinished mourning.
For most people, disappointments or worries can trigger the mildest form of depression commonly called the “blues” or the “blahs.” These gloomy moods often respond to simple interventions, departing as quickly and sometimes as mysteriously as they arrived. Not so with grief — the overwhelming sorrow
that accompanies the death of a spouse or a beloved pet, or a decline in health. Usually, over time, grief gradually diminishes. The mourner experiences shorter periods of intense feelings alternating with longer periods of better mood, but it may take a year or more before the worst is over.
For elderly people, mild disappointments and grief can set off depression. According to estimates from the National Institute of Mental Health, nearly 750,000 older Californians suffer from depression each year. Put in another way, 50 percent of all seniors will endure a depression at some
point in their later years.
Depression can affect the entire family — but the family can also help intervene.
Washing the Blues Away
Engaging mom or dad in activities that they enjoyed in the past can often shoo away — or at least speed up — the demise of the blahs. A simple thing, like arranging a visit from a favorite grandchild or a close friend, can be effective, too.
You might try appealing to your parent’s “child within” by preparing a bubble bath or reading to him her, or putting on an old slapstick comedy and making popcorn for you to share. Inviting a senior who is in a funk to help you with your gardening, dish drying or sorting socks allows him or her
to contribute to the upkeep of the household while being distracted from his or her own low feelings.
Research demonstrates that mild or moderate exercise also has depression-lifting benefits.
Managing Grief
When the death of a loved one is the reason for the sadness, acknowledge the loss in as many ways as possible. Call frequently, send notes, visit and honor the departed with donations or memorials. Mention the deceased, recalling his or her special moments and pleasing personality traits. Talking
lessens the pain. Understand that your parent’s anger (directed at clergy, the doctor, God, the rescue teams and you) is likely to be a only a temporary stage in the grieving process. Don’t take it personally or argue about it.
Encourage your parent to find solace in spiritual, cultural, and religious practices. Provide extra attention during the anniversaries, birthdays and holidays that fall during the first year after the loss. Don’t discourage crying or suggest that she “ought to be over it by now!” Comments
like: “At least he’s not suffering any more” or “At least he lived a long life” do not help. Instead of saying “Call me if I can do anything,” make specific offers, such as “Can I pick up the groceries or cook dinner tonight?”
It’s extremely helpful to tell your grieving parent that anyone in the same position would be in similar emotional pain.
Healing Through Reminiscence
The older people get, the more time they spend reflecting on the past. This is a good and healthy thing to do. Reminiscence brings the past into the present and reminds an older person that he isn’t just an old man — he’s been a father, a businessman, a teacher and a darn good golfer. He is
loved and admired.
Should the remembering be filled with sorrow or regret, remind your mother that she probably did the best she could with what she had available at the time.
You can foster positive reminiscence by suggesting that your parent record his or her memories in a journal.
Work together on a scrapbook with photos, newspaper clippings, letters, postcards, greeting cards, sketches and poetry.
Create a video or audio recording of stories highlightingall of your father’s accomplishments and happiest moments.
Healing Through Igniting Interest in Others
Jim W., a 75-year-old widower who lives in the San Fernando Valley, struggled with depression for years, until he got all fired up about the city’s plan to bring down a half-dozen magnificent old trees. He quickly became too busy organizing sit-ins and protests to dwell on himself and his
losses.
Any time you can redirect your parent’s attention outward — even for a short time — you have made an inroad. Gently convince, cajole and persuade your parent to stay involved in the lives of family and friends, participate in a support group, or volunteer.
Recognizing Clinical Depression
Clinical depression is a deep melancholy that persists over weeks and months. It can become so severe that the senior’s health deteriorates as his ability for self-care becomes compromised.
A medical evaluation can determine whether illness or drug side effects are contributing to the problem. Once the doctor rules out those possibilities, he or she may suggest therapy with a trained therapist who can help the older adult gain a more optimistic view of life, enhance his coping
skills and put to rest things that have troubled your parent for decades.
Taking Medicine
Depression is an illness, not a character flaw. Don’t let your parent resist visiting the doctor for depression because he believes that he should be strong enough to overcome it himself.
Antidepressants for severe depression are effective in 80 percent of patients. Unfortunately, as discovered in a recent UCLA study, fewer than one in three depressed seniors had received treatment for their depression in the previous three months. Antidepressants generally take about two weeks to
begin to take effect, and it may be as many as four to six weeks before the elder feels better. In the meantime, therapy can help your parent learn more successful ways to deal with life’s problems. Most people do best on a combination of talk therapy and antidepressants. (In some cases, electroconvulsive therapy or “shock therapy” may be recommended. It sounds frightening, but nowadays it’s quick, effective and safe — and especially successful in treating elderly people whose depression doesn’t respond to any other treatment.)
Where to Turn for Help
Jewish Family Service (JFS) of Los Angeles operates five senior centers. All five offer counseling.
“We do not believe that depression is an inevitable part of aging,” said Karen Leaf, director of the JFS Valley Storefront Senior Center. “We feel that older adults who are depressed can greatly benefit from individual and group psychotherapy.”
JFS offers groups for widowers, seniors with difficult relationships with adult children, caregivers (who are at high risk for depression) and general for-men-only or for-women-only groups.
Leaf urges adult children to be aware of depressive signs and be willing to suggest counseling to a depressed aging parent. She advises children to “speak from the heart” with “I” statements. For example, “Mom, I have observed that you are very sad and are losing weight. There’s a Jewish
organization that can help. People need some help from time to time, and you have a lot of things on your plate.”
If your efforts to get your parent into treatment are unsuccessful, Leaf cautioned, “You have to let it go, because ultimately, unless their safety is at risk, there are boundaries that must be respected.”
For more information on Jewish Family Service, call (323) 761-8800, to find the nearest center. Sometimes Medicare will cover the fee. If not, don’t worry — JFS operates on a sliding-fee scale.
The Center for Healthy Aging (CHA) in Santa Monica also provides help to depressed seniors and their families. CHA’s services include individual psychotherapy, group therapy and medication management.
There’s also senior peer counseling — a model program that has been replicated throughout the United States and abroad.
The program trains volunteer senior peer counselors to help other older adults over the rough spots. Peer counseling is ideal for depressed seniors who need emotional support but may be uncomfortable with the idea of using mental health professionals and services, yet are willing to talk to
counselors they perceive as more like themselves (for example, widows and former caregivers).
If your parent lives on the greater Westside and is reluctant to call CHA, you may call Dr. Amy Liston, at (310) 576-2550 ext. 217. CHA provides supportive services to the adult child and their elderly parent. There is a sliding fee scale.
The Los Angeles Jewish Home for the Aging (JHA) employs geriatricians that are available to see their resident patients as frequently as necessary.
Laurie Manners, administrator of Grancell Village of JHA, explained that JHA works closely with a geropsychiatric group that provides both psychiatrists and psychologists. These mental health professionals address elder depression and other psychiatric needs for the JHA’s residents each week,
and are available for emergency services. Residents are helped using a variety of treatments (including behavior modification, one-on-one counseling, medication or a combination of these).
“We treat depression aggressively whether it comes from grieving, life events or transitions or other general living issues,” Manners said.
For more information about the Los Angeles Jewish Home for the
Aging call (818) 774-3306.
How to Recognize Clinical Depression
If your elder exhibits any of the following symptoms, he or she may be suffering from a clinical depression and should be seen by a physician:
- Describes a feeling of “emptiness” or “hopelessness”
- Shows lack of interest in everyday activities
- No longer enjoys formerly pleasurable pastimes
- Cries often, sometimes for no apparent reason
- Complains about lack of concentration, faulty memory and trouble making decisions
- Expresses feelings of worthlessness or guilt
- Has thoughts of suicide or has made an attempt
- Complains of headaches, backaches or stomachaches that don’t respond to treatment (when physical problems hide depression, the condition is called a masked depression)
- Uses more alcohol, drugs and tobacco
- Pays less attention to grooming and hygiene
- Sleeps too little or too much, has trouble falling asleep and may wake up early, unable to fall asleep again
- Appears tired and sluggish
- Eats more or less than usual, resulting in significant
weight gain or loss - Frequently becomes agitated, hostile, or disoriented
- Adopts depressive positions and gestures (including sad
facial expressions, being stooped over and staring across the room)
Dr. Rachelle Zukerman is professor emeritus at UCLA, a gerontologist, author of “Eldercare for Dummies” (Wiley Publishing) and a public speaker on aging issues. She can be reached at DrRZuk@aol.com.



















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.