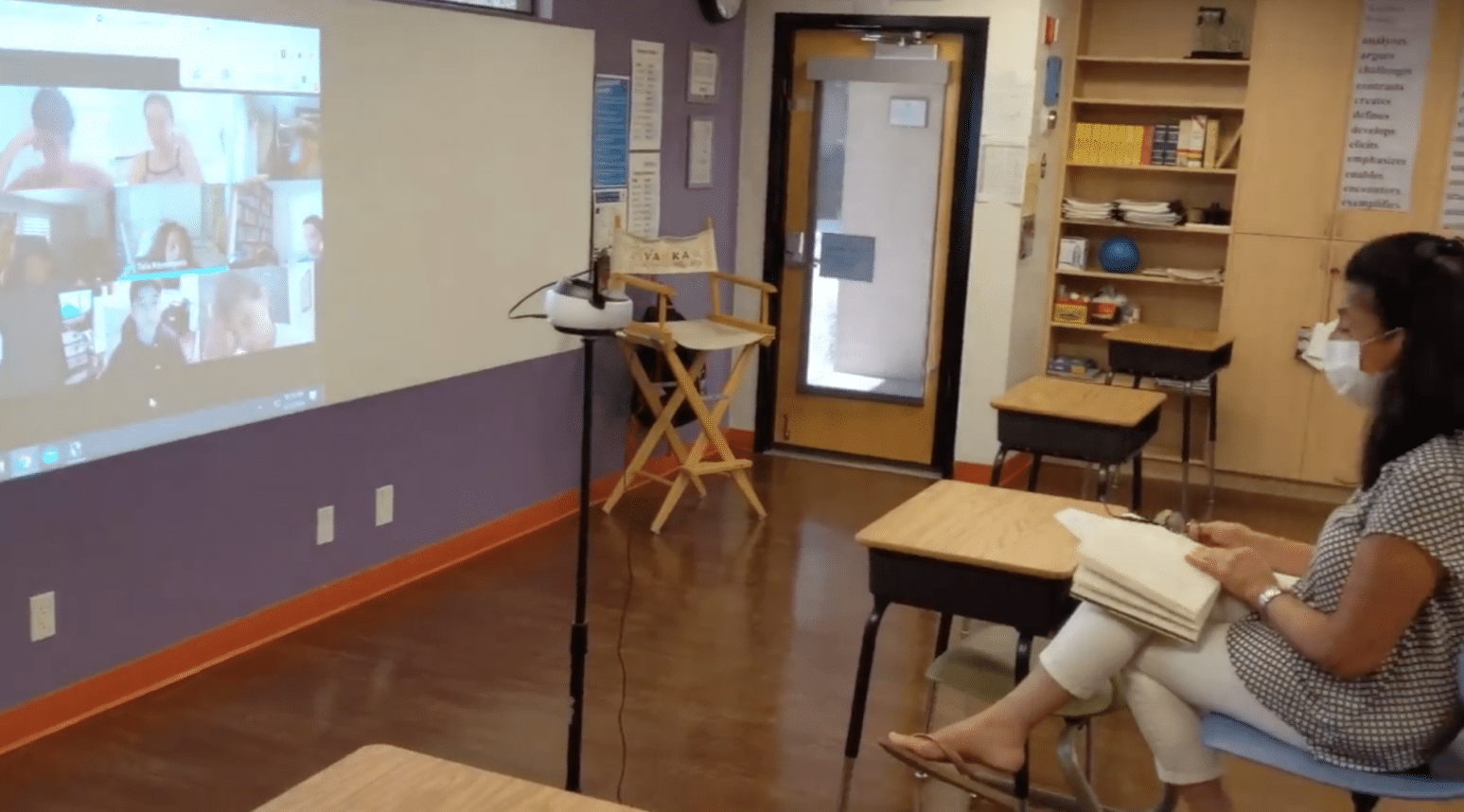
Back to School 2020: Local Jewish Day Schools Have Plans for Both Distance and In-Person Learning
Principals and administrators have spent much of the summer ironing out multiple plans to return, whether in-person, online, or some combination of the two.










 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.