It’s the fourth deadliest cancer, which will claim an estimated 34,000 lives this year. There are no surefire methods for prevention or early detection. And it resists treatments found to be effective in other cancers.
Until someone noteworthy like U.S. Supreme Court Justice Ruth Bader Ginsburg or actor Patrick Swayze is diagnosed with it, pancreatic cancer tends to keep a low profile.
Funding for pancreatic cancer research lags far behind that for breast or prostate cancer, even after the National Cancer Institute increased its spending by 20 percent last year. Despite the obstacles, local physicians and researchers are looking for better treatments and showing hints of optimism about potential progress against this disease, which strikes Jews with greater frequency than the general population.
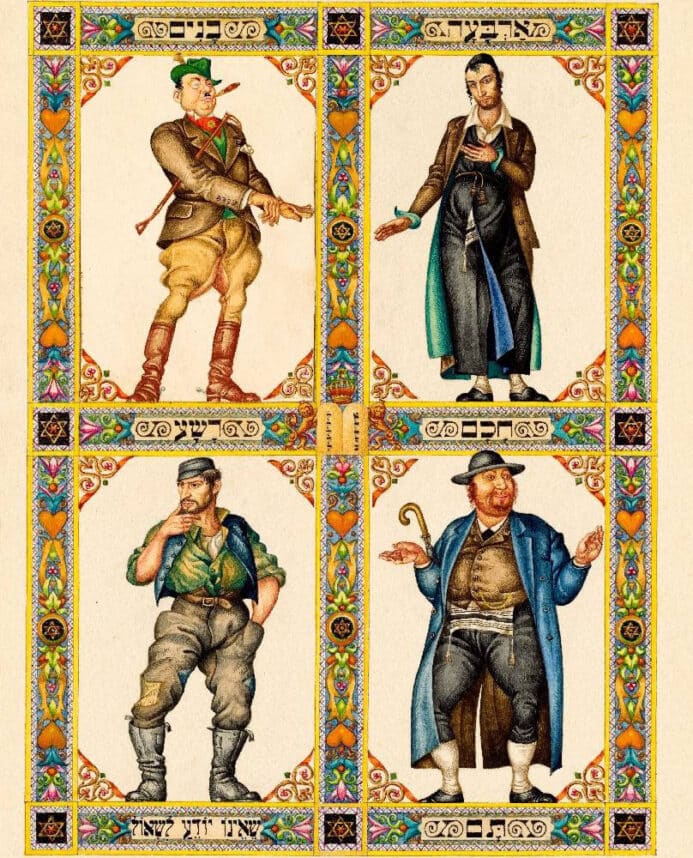
The location of the pancreas — a pear-shaped gland tucked between the stomach and spine that aids in digestion and produces several hormones, including insulin — makes it difficult for physicians to see or feel masses during routine exams. Risk factors include a history of chronic pancreatitis, cigarette smoking, obesity or long-standing diabetes. And although the majority of cases are not hereditary, certain hereditary conditions (including Ashkenazic genetic mutations, like BRCA2) are associated with pancreatic cancer.
Pancreatic cancer frequently has no early symptoms, so the disease is typically diagnosed in advanced stages.
Attacking the Cancer
Physicians at UCLA participating in a Phase II clinical trial are testing a vaccine designed to stimulate the body’s immune response to cells that have undergone genetic changes associated with pancreatic cancer. The trial targets patients who have already undergone surgery.
“The idea is to teach the body to kill only the cells with the mutations,” said Dr. Edward Garon, an assistant professor of medicine with the UCLA David Geffen School of Medicine’s division of hematology/oncology. “We don’t know if it will be successful, but the hope is that we can reduce the likelihood of recurrent cancer.”
Another UCLA trial is looking to gene therapy to make tumors more susceptible to the effects of chemotherapy and radiation by rendering them vulnerable to inflammation. The hope for this Phase III trial is to more effectively kill cancer cells so patients with an advanced form of the disease can subsequently undergo surgery.
Researchers are also looking for substances to help boost the effectiveness of standard pancreatic cancer therapy, a drug called gemcitabine (marketed as Gemzar by Eli Lilly and Co.).
“This has been a frustrating area,” said Dr. Steven Miles, a medical oncologist at the Samuel Oschin Comprehensive Cancer Institute at Cedars-Sinai Medical Center. “Gemcitabine itself was approved [by the FDA in 1997] after showing that patients live four months longer than the previous therapy. Despite numerous randomized trials testing different agents paired up with gemcitabine, only one showed positive results, and it only extended life by 14 days. Some patients had great response, and others showed none.”
Miles noted that treatment is becoming more individualized. Different chemotherapy drugs target different proteins associated with cancer. Since tests can now determine which proteins are elevated in an individual patient’s cancer, physicians can better predict which drugs would be most effective in that patient’s case.
The individualized approach is also driving research. “We are trying to identify genetic signatures that might help develop new drugs and targets,” said Dr. J. Randolph Hecht, professor of clinical medicine and director of the UCLA Gastrointestinal Oncology Program. “The one-size-fits-all approach to pancreatic cancer clearly has failed.”
Another focus of research involves analyzing how normal pancreas cells transform into cancerous ones.
“The idea is to attack the cancer before it starts, rather than after it has spread,” said Joseph Kim, assistant professor of surgery at City of Hope.
Improving Screening
UCLA is also participating in the Cancer of the Pancreas Screening Study (CAPS 3), which screens individuals who have multiple relatives with pancreatic cancer or who have gene mutations associated with the disease.
The study hopes to find proteins that indicate pancreatic tumor development and to develop an effective method of locating tiny pre-cancerous pancreatic lesions so they can be treated before developing into cancer.
Barriers to Progress
“We’re seeing more clinical trials than ever before. Still, we haven’t had a major breakthrough,” said Michelle Duff, director of research and scientific affairs for PanCAN (Pancreatic Cancer Action Network), a national organization promoting research, patient education and support.
Duff said pancreatic cancer is underfunded, noting that the National Cancer Institute, a co-sponsor of the CAPS 3 study, devoted $87 million for research into pancreatic cancer last year, compared to $237 million for colorectal cancer, $572 million for breast cancer, and $285 million for prostate cancer (the second, third and fifth highest mortality cancers, respectively).
UCLA’s Hecht noted that only 5 percent of all cancer patients nationwide are enrolled in clinical trials, and he would like to see that number increase.
“Clinical trials increase survival and quality of life,” he said. “They are the only way to improve the outcome of this terrible disease.”
Hope for the Future
While the statistics are bleak, the researchers interviewed remain optimistic.
“I strongly believe that with a strong research program, followed by well-conducted clinical studies, we will be able to make substantial progress in the treatment of pancreatic cancer,” UCLA’s Garon said.
“We don’t know where the next treatment advance might come from,” Cedars-Sinai’s Miles said. “Being alive with AIDS in August of 1995 versus September of 1995 meant the difference between death and survival. Because that’s when a new drug completely transformed treatment. The same thing could happen for pancreatic cancer.”
For more information about pancreatic cancer treatment and research, call PanCAN’s Patient and Liaison Services at (877) 272-6226 or visit http://www.pancan.org/.



















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.