
Category
tumor

Going along hand in hand
Jewish Journal
September 24, 2013
Twenty-three years ago, Lisa Szilagyi gave birth to her first child, Emily, who was diagnosed with tuberous sclerosis, a genetic disease that causes tumors to grow on vital organs. It resulted in severe epilepsy and essentially made Emily nonverbal.
Jailed Alan Gross may have tumor, doctor says
Jewish Journal
October 3, 2012
Jailed Alan Gross may have tumor, doctor says
EU’s Ashton condemns ‘hateful’ Iran remarks on Israel
Jewish Journal
August 21, 2012
The EU foreign policy chief said on Saturday that comments by Iranian President Mahmoud Ahmadinejad, who called Israel a \”cancerous tumor\” with no place in a future Middle East, were \”outrageous and hateful.\”
Can MRI save lives?
Adam Wills
October 5, 2006
MRI is increasingly being recommended as a complimentary screening tool, especially to find invasive tumors.
New Articles

BRAVE-ish on ReachTV Where Next!
Lisa Ellen Niver
April 25, 2024

On Counting the Omer
Rabbi Dr. Stuart Halpern
April 25, 2024
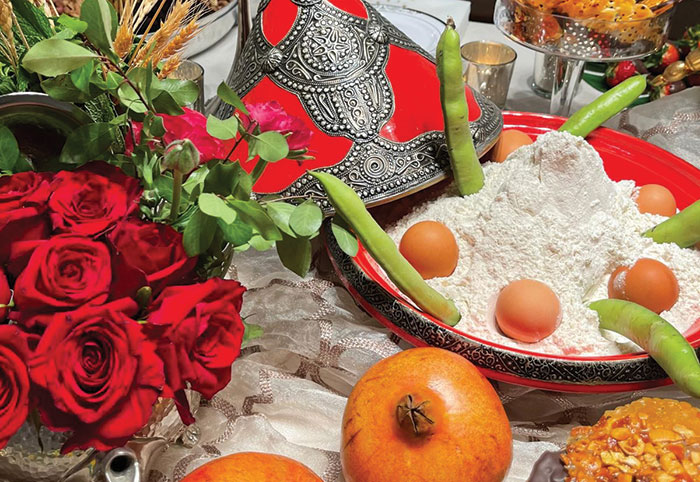
A Memorable Mimouna
Sharon Gomperts and Rachel Emquies Sheff
April 25, 2024

Campus Watch April 25, 2024
Aaron Bandler
April 25, 2024

Will Columbia’s Law School Dean Learn the Law of Free Speech?
Nathan Lewin, JNS
April 25, 2024
 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.