Category
transplant
Bone Marrow: The best kind of gift
In 2002, Los Angeles native Ronnel Conn was an undergraduate at George Washington University in Washington, D.C. When he heard there would be a bone marrow donor drive at the campus Hillel for a D.C. local in need, he showed up and got his cheek swabbed, because, he said, “It seemed like the right thing to do.”
Awaiting transplant, family rallies with hope
Michael Goldberg’s heart is working just fine. The University of Washington professor teaches a class on romantic comedies. From “Annie Hall” to “Pretty Woman,” he leads his students on a tour of film’s fondest genre.
A Kidney for Chana
Chana Bogatz is 5 years old, and she loves cutting and pasting paper, playing with her brothers and sisters and having \”Happy Birthday\” sung to her.
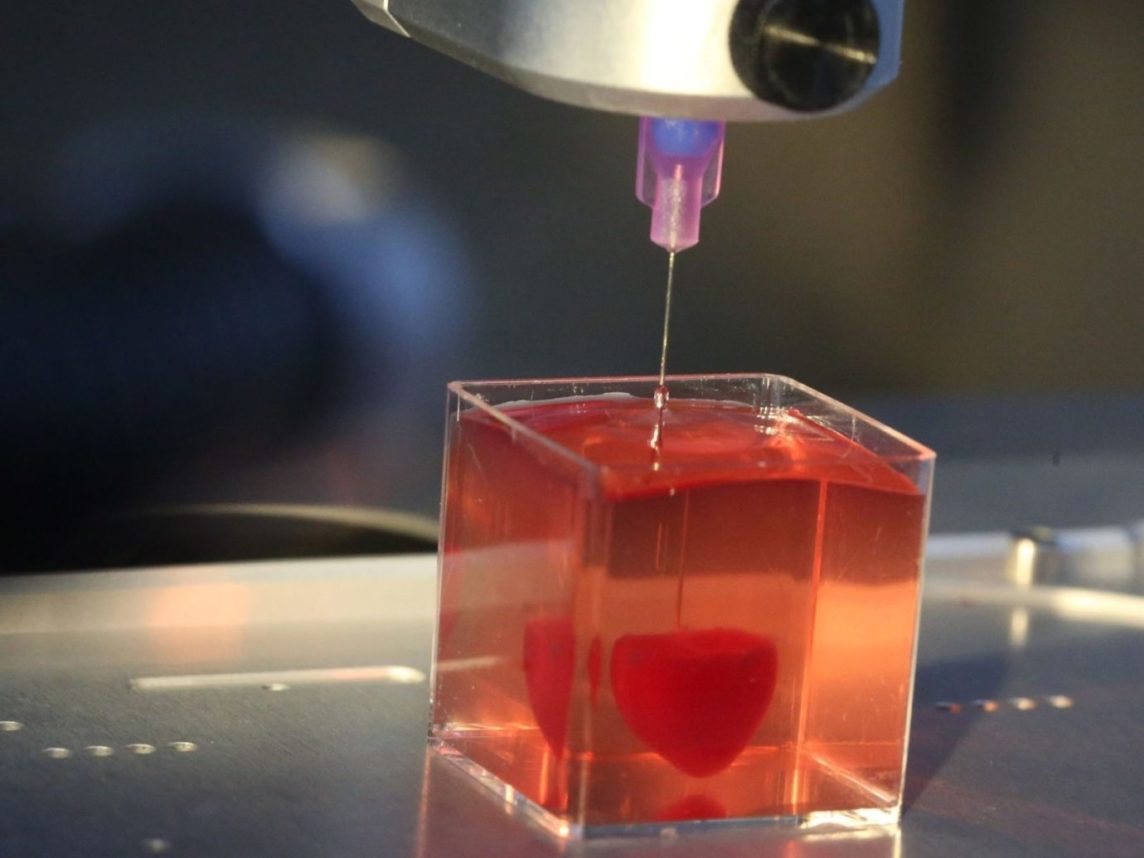
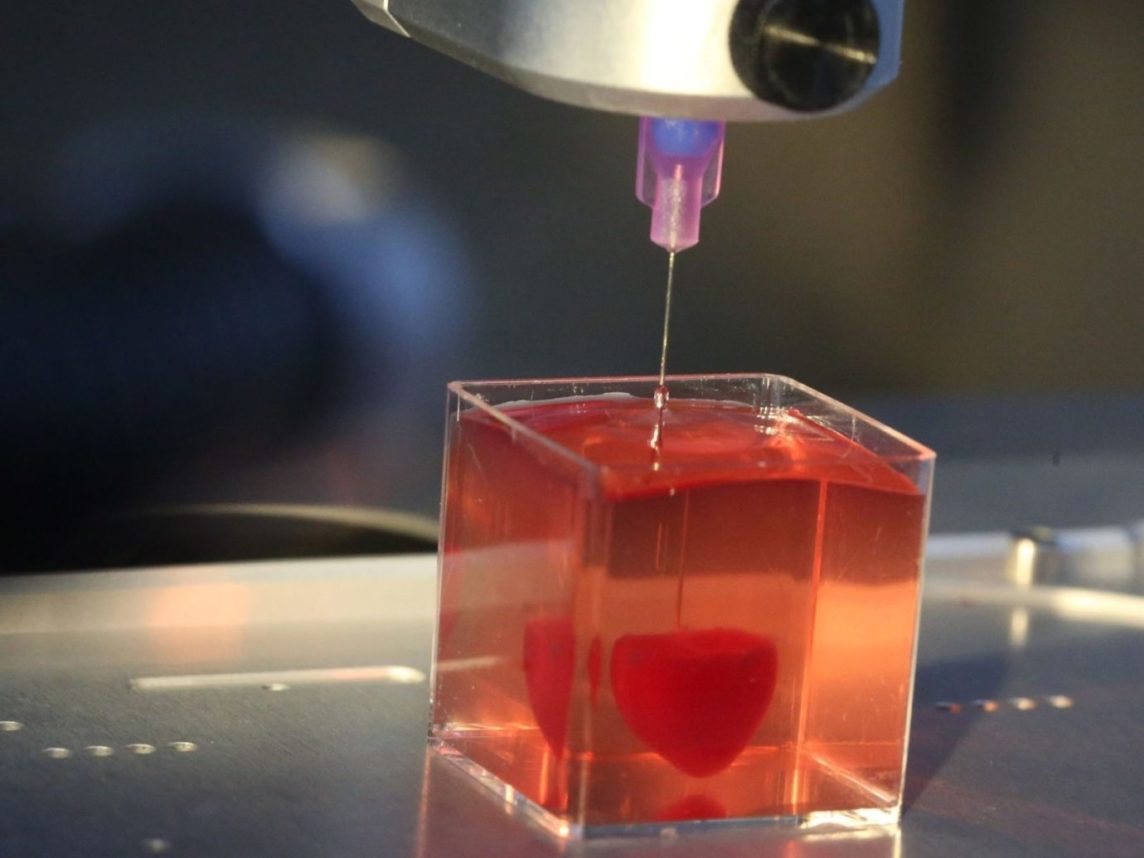
Just the Right Size
This is a heartwarming story about a kidney.
The kidney in question belongs to Mike Jones. It used to belong to Patricia Abdullah.
Jones and Abdullah have very little, apparently, in common. Jones is an African American man. Abdullah is a female descendant of the Hawaiian royal family. Jones is Christian. Abdullah is Muslim. Jones lives in the city. Abdullah lives in the Valley.
They\’re a perfect match. Sometimes you just have to stay positive. O-positive.
History in the Making
By the time the transplant team approached Doris Ullendorf and Ken Gorfinkle, they had already talked about donating the organs of their first-born son.
New Articles

Print Issue: Sitting With Rebels | April 19, 2024

Oct. 7 Events to Be Depicted in New Stage Show

Shani Seidman: Manischewitz, Passover Memories and Matzo Brei

Rabbis of LA | Rabbi Robbie Tombosky Lives in Two Worlds That Really Are One
 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.