Beyond book smarts: What this international medical school gives future doctors
For most pursuing a career in medicine, the long-haul investment in studying, training and preparing to become a physician is the fulfillment of a lifelong dream.
For most pursuing a career in medicine, the long-haul investment in studying, training and preparing to become a physician is the fulfillment of a lifelong dream.
A Palestinian Authority minister of health visited Hadassah Hospital in Jerusalem reportedly for the first time.
Thirty-eight physicians from Europe wrote a paper alleging that “cultural bias” was behind the pro-circumcision stance of the American Academy of Pediatrics.
Sometimes, adversity strikes gold. In Los Angeles, three major medical institutions, including Cedars of Lebanon and Mount Sinai — the independent hospitals that merged to form Cedars-Sinai Medical Center — and the City of Hope sprang from Los Angeles\’ Jewish tuberculosis problem.
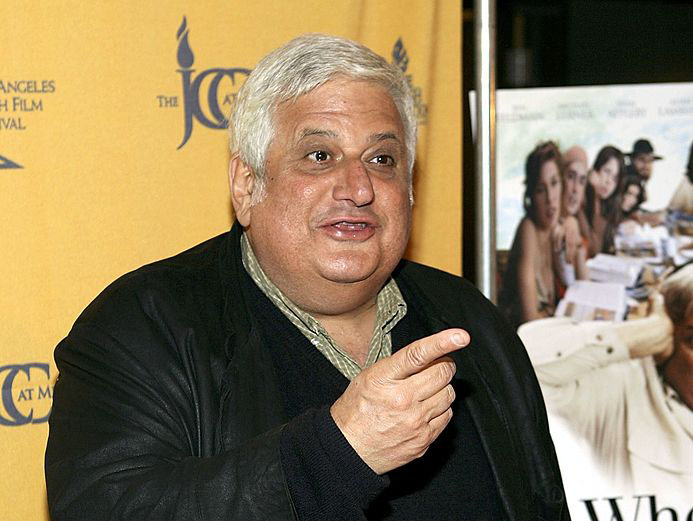
Physicians played a significant role in the Holocaust, and today\’s doctors can learn from the ethical failures of that period, according to an article recently published by Dr. Joel Geiderman, co-chair of the emergency department (ED) of Cedars-Sinai Medical Center.
In \”Physician Complicity in the Holocaust: Historical Review and Reflections on Emergency Medicine in the 21st Century,\” Geiderman sets out a series of moral failures he attributes to German physicians before, during and after WWII. Published in the March issue of Academic Emergency Medicine journal, the two-part article enumerates ethical challenges requiring greater vigilance from today\’s physicians.




 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.