
E Pluribus Unum: Doctors Taking on COVID-19 Together
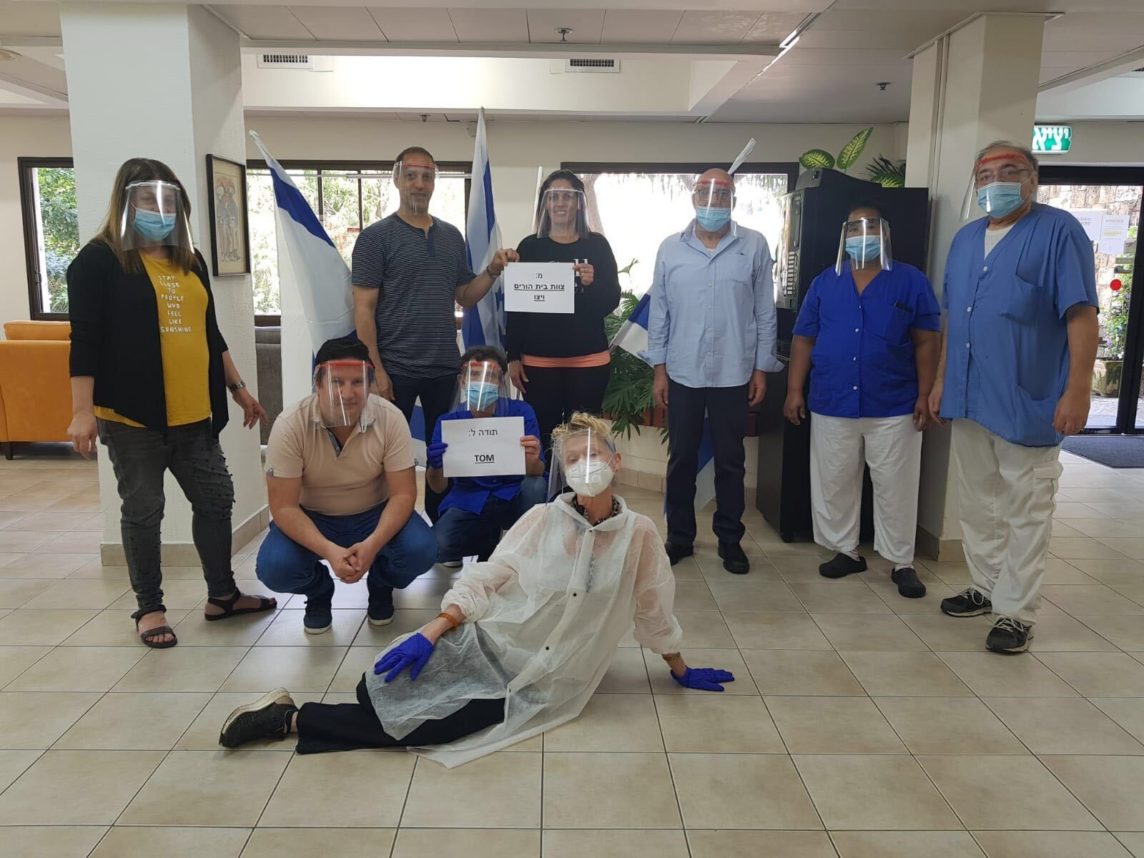
Our doctors, nurses and pharmacists successfully restructured health care so effectively because we looked first to the needs of patients and colleagues rather than our own.

Our doctors, nurses and pharmacists successfully restructured health care so effectively because we looked first to the needs of patients and colleagues rather than our own.
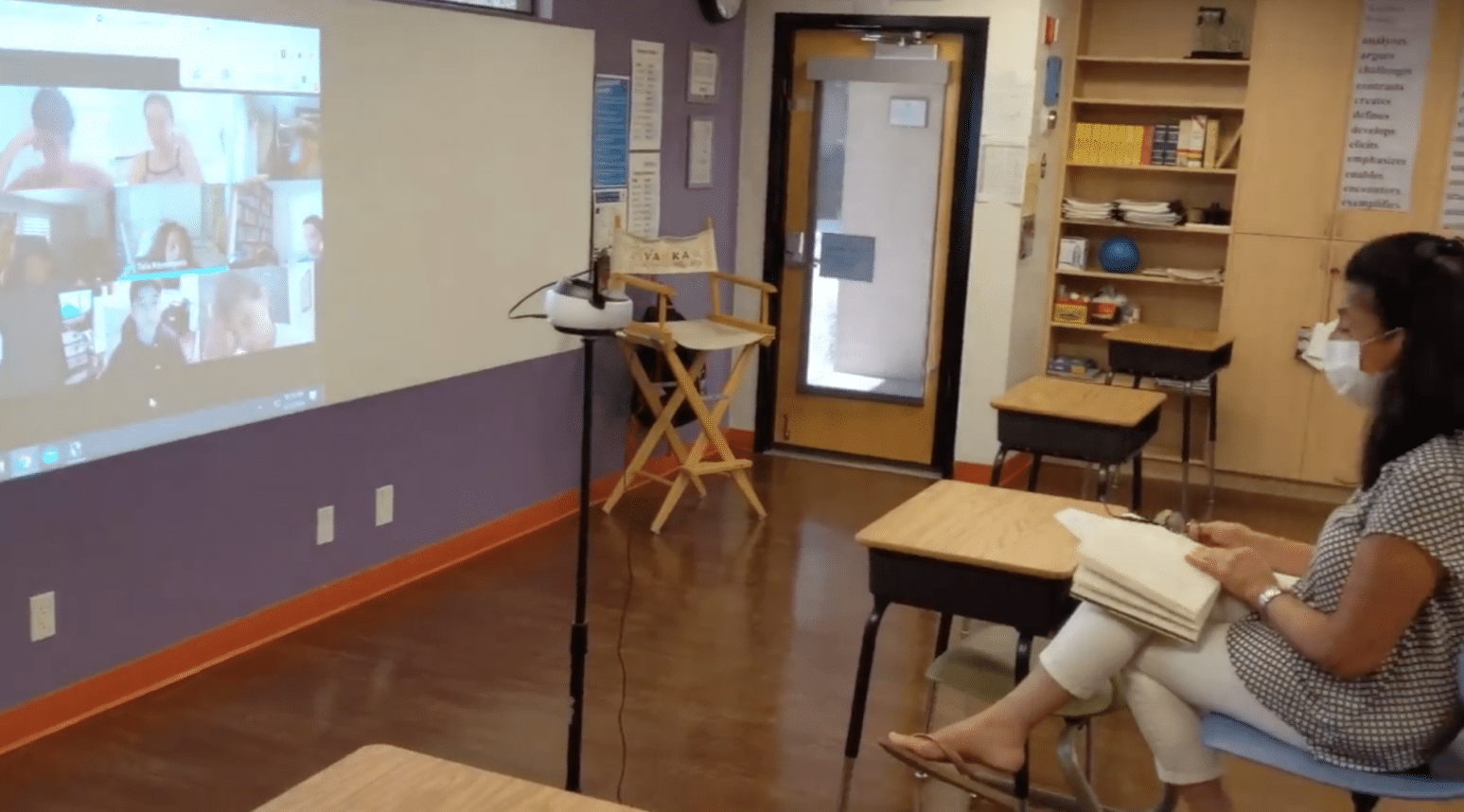
Principals and administrators have spent much of the summer ironing out multiple plans to return, whether in-person, online, or some combination of the two.

“Being able to deliver and get them what they ask for is wonderful. We’re letting them know that they’re not alone.”
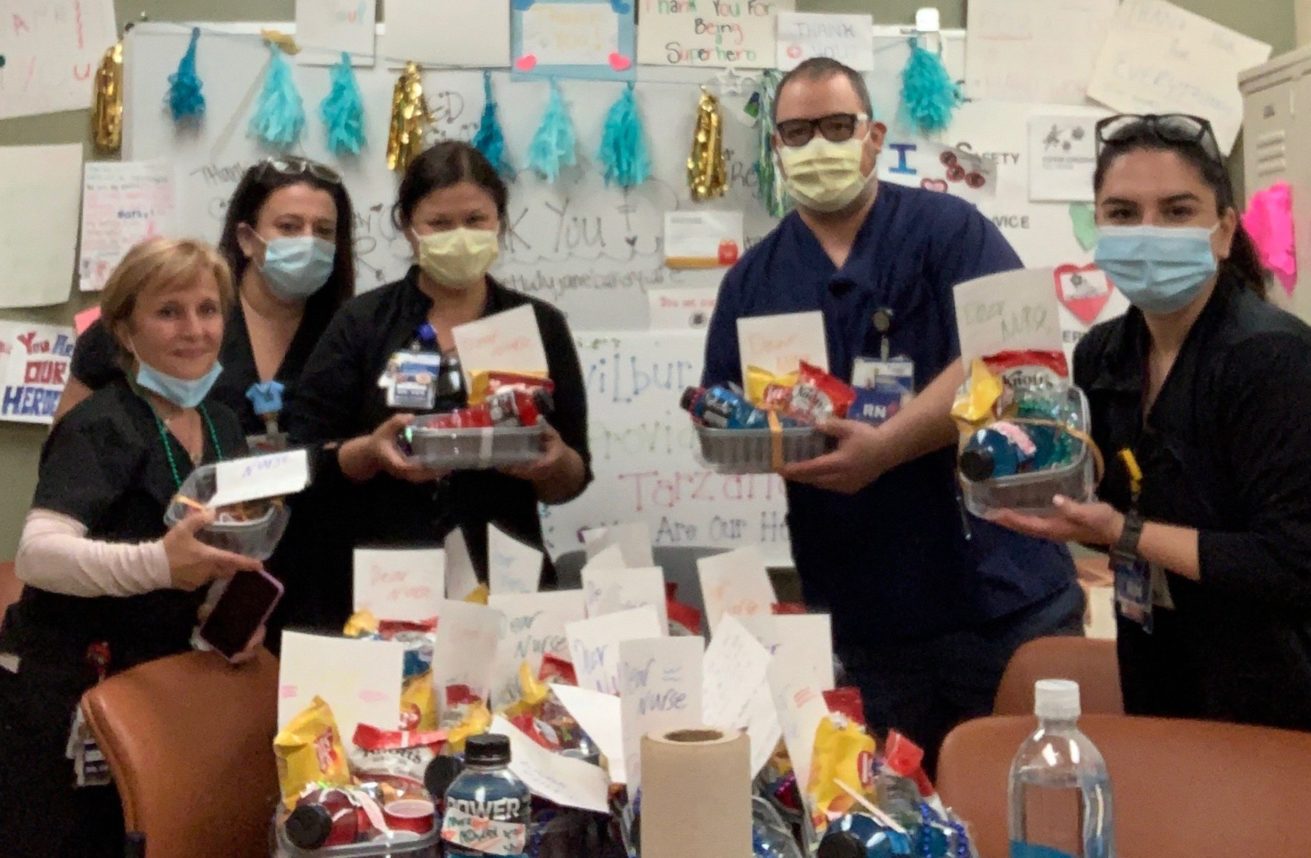
“Receiving all these generous donations from businesses and families remind us, too, that they are rooting for us, and we are all in this together.”

Wearing masks is crucial for public safety, especially as we reopen our economy.

The Journal spoke with 62-year-old Rik Heller, the Dallas-based inventor of welloStationX, about his device.





 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.