
Category
doctors


Beyond book smarts: What this international medical school gives future doctors
For most pursuing a career in medicine, the long-haul investment in studying, training and preparing to become a physician is the fulfillment of a lifelong dream.
Fake medicine
Caveat emptor means “buyer beware.” Fake medicines are now a multibillion-dollar industry affecting people in virtually every country in the world, and the problem is getting worse. It has been estimated that up to 15 percent of drugs sold worldwide are counterfeit, and in parts of Africa and Asia it can surpass 50 percent. We are also vulnerable in the United States even though we have a better-regulated pharmaceutical system.
Israeli medical residents say they’ll ignore back-to-work order
Hundreds of Israeli medical residents who resigned said they will not obey an order by the National Labor Court sending them back to work.
Czech Republic: Doctors’ Group Apologizes to Jews
A Czech doctors’ organization apologized to Jewish doctors Thursday for the persecution they endured in pre-World War II Czechoslovakia, an official of the organization said. In October 1938, before the Nazis invaded, organizations of Czechoslovak doctors, lawyers and others issued a memorandum urging the government “to take energetic measures” to prevent Jews from practicing. “We apologize for what our predecessors did to you,” stated a document by the Czech Medical Chamber in Prague. Many Jewish doctors lost their jobs when the government banned them from working in state institutions. The Czech bar association issued a similar apology a year ago.
Ashkenazi women and ovarian cancer
Dr. Beth Y. Karlan is the director of the Cedars-Sinai Women\’s Cancer Research Institute at the Samuel Oschin Comprehensive Cancer Institute. Her specialty is ovarian cancer, the deadliest of gynecologic cancers and one that is diagnosed in more than 22,000 women annually.
Get the doctor’s attention — for a fee
Rising costs, crowded waiting rooms and decreasing access to doctors are among the reasons medical patients in Southern California and across the nation use words like \”headache\” and \”frustration\” to describe America\’s health care system. And with declining insurance reimbursements, rising malpractice premiums, claims frustrations and growing paperwork, individual practitioners are often forced to increase the volume of patients they see as they decrease time spent in the examination room.
Veggie lovers could fare better in cancer fight
New and better information is coming to light every day about ways to prevent this common disease. Since doctors are getting better at catching it early, fewer men are dying of prostate cancer. But one in six men will still develop the disease in their lifetime.
Doctor with ‘healing hands’ helps kids from Iran to L.A.
When Ralph Salimpour was six years old in Esfahan, Iran, he had malaria — a blood disease spread by infected mosquitoes that kills millions of people in the developing world every year.
New Articles

NSFW – A Poem for Parsha Metzora

Israel War Room Launches in Spanish
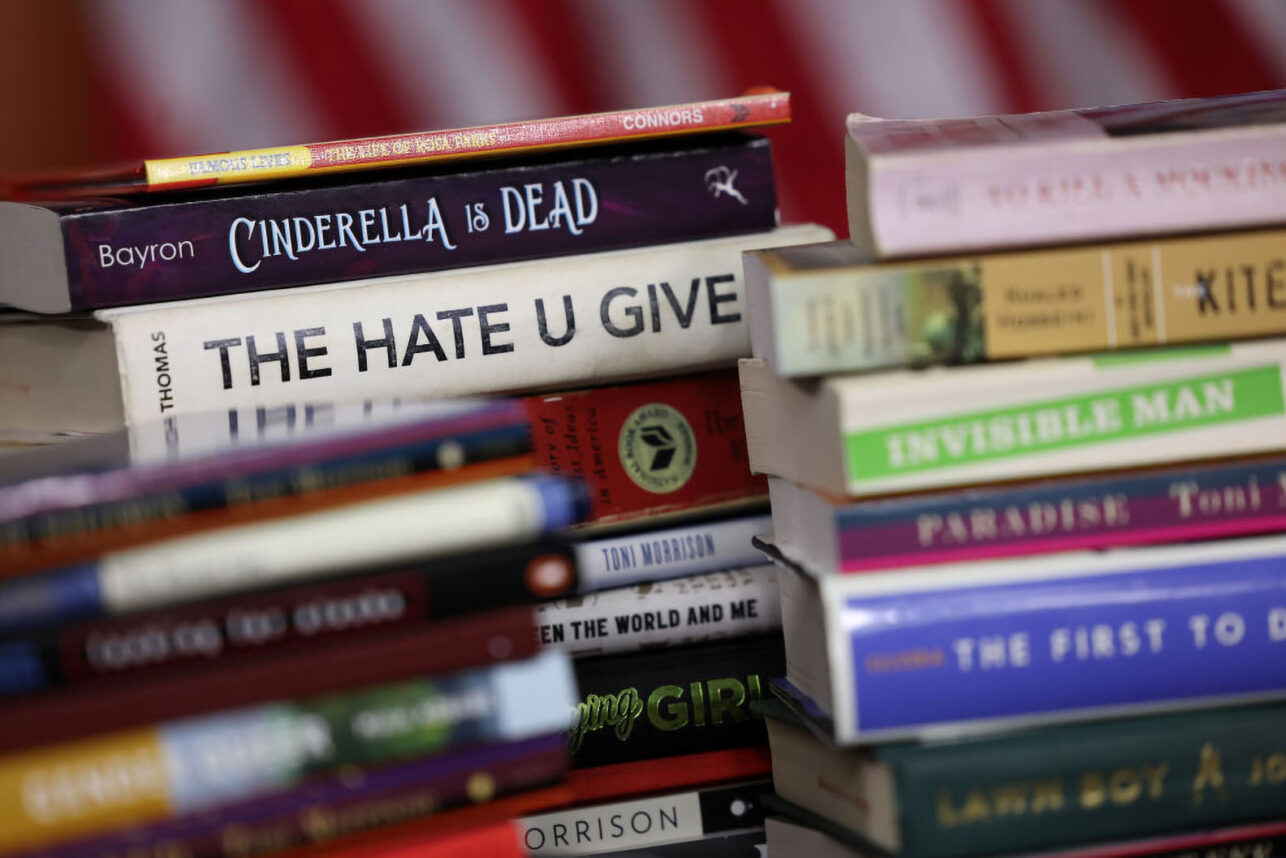
Modern Book Bans Echo Past Atrocities and Further Silence Marginalized Voices

The Power of the Passover Seder to Unite Jews
 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.