
Category
disease


Seven Day Quarantines Were So Quaint – a poem for Torah Portion Tazria-Metzora
Rick Lupert
April 23, 2020

Coronavirus: How to Keep Things in Perspective
Ignacio López-Goñi, World Economic Forum
March 11, 2020




‘Nightmare bacteria,’ shrugging off antibiotics, on rise in U.S.
Jewish Journal
March 5, 2013
\”Nightmare bacteria\” that have become increasingly resistant to even the strongest antibiotics infected patients in 4 percent of U.S. hospitals in the first half of 2012 and in 18 percent of specialty hospitals, public health officials said on Tuesday.
Persian Tay-Sachs
Jewish Journal
December 1, 2011
In the story, a young prince in an old and distant kingdom is mesmerized with salt.
When prostate cancer scare hits close to home
Jewish Journal
November 2, 2011
When Rabbi John Rosove of Temple Israel of Hollywood was diagnosed with prostate cancer in 2009, he was devastated. Given a dire prognosis by his first doctor (who later turned out to have exaggerated the circumstances), he felt the weight of his own mortality for the first time.
New Articles

Israel Strikes Deep Inside Iran
Charles Bybelezer, JNS
April 19, 2024

NSFW – A Poem for Parsha Metzora
Rick Lupert
April 18, 2024

Israel War Room Launches in Spanish
Kylie Ora Lobell
April 18, 2024
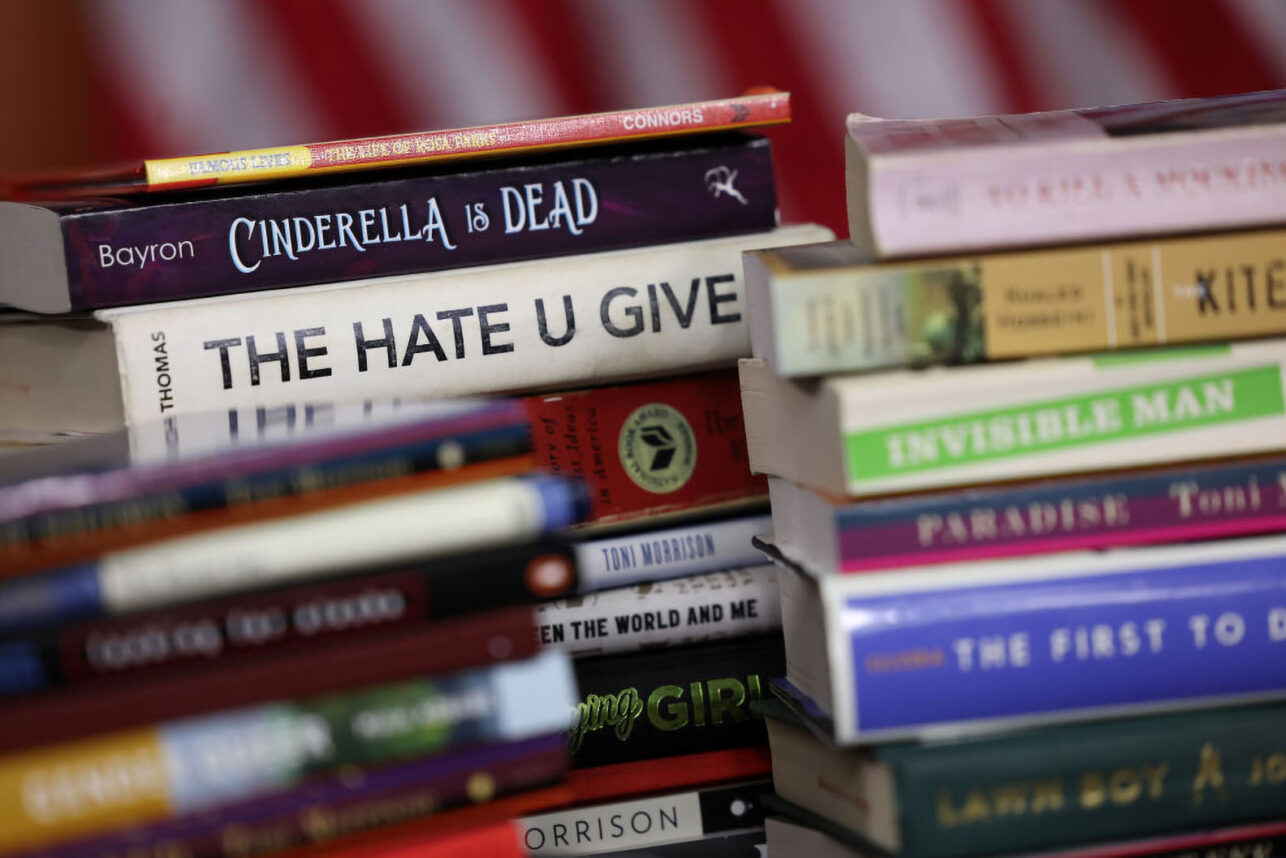
Modern Book Bans Echo Past Atrocities and Further Silence Marginalized Voices
Larry Bailis and Cindy Rowe
April 18, 2024

The Power of the Passover Seder to Unite Jews
Samuel J. Abrams
April 18, 2024
 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.