
Category
dementia

In life-or-death legal dispute, modern medical ethics, Jewish law and civil law clash
As David Stern, 61, an observant Orthodox Jew suffering from a rare neurodegenerative disease, lies conscious and hooked up to a respirator at the Providence Tarzana Medical Center in the San Fernando Valley, the hospital and lawyers for two of Stern’s children are battling to determine whether the hospital should remove Stern from life support
Swinging with The 5th Dementia
Twice a week, four older men get together to make music. There may be nothing unusual about that, but aging has not been kind to them: To varying degrees, they’ve been affected by dementia or Parkinson’s disease.\n
The emotional landmines of family caregiving
A painful situation for the primary caregiver occurs when another close relative does little or nothing to help, but they are adored and praised by the senior anyway.
Films: Dementia ordeal inspires comic tale of ‘The Savages’
Tamara Jenkins knows firsthand what an overwhelming task it is to care for a parent suffering from dementia. While she was in her mid-30s, she had to help care for both her father and grandmother during their final days in a nursing home. She also knows that no matter how grave a situation might be, there are always sparks of humor surrounding it. So it\’s no surprise that her new film, \”The Savages,\” addresses that very subject and does so with a healthy dose of comic perspective.
Center’s Studies Aid Care for Frail Elderly
Weight-loss prevention is one of the principal areas of investigation at the Borun Center, a joint venture between JHA and UCLA\’s David Geffen School of Medicine. Housed on the JHA campus in Reseda, the center was established in 1989 to identify and test nonmedical measures that could improve daily care and quality of life for nursing home residents.
A Big Impression
My senior students suffer from short-term memory loss, a condition less severe than Alzheimer\’s and dementia but nonetheless frightening. They can recall exact moments from decades past, but in the present, from one moment to the next, many don\’t remember who or where they are. Sort of like elected officials.
Problems Abound in Pampering Parents
My mother and father are both in diapers. I wasn\’t at all prepared for this possibility. Dealing with the visual and olfactory aspect of my son\’s end products when he was a baby was an expected part of being a mom, but it\’s a completely different matter when it\’s my parents wearing the Pampers.
Elder Rage: What I Know Now
For 11 years. I begged my obstinate elderly father to allow a caregiver to help him with my ailing mother, but he adamantly insisted on taking care of her himself. Every caregiver I hired to help him said, \”Jacqueline, I just can\’t work with your father — his temper is impossible to handle. I don\’t think you\’ll be able to get him to accept help until he\’s on his knees himself.\”
Mom and Dementia
I reminded Mom of her move to Los Angeles three years ago, and her life at a San Fernando Valley board and care.
She sighed and said, \”Ellie, I\’m losing my marbles.\”
New Articles
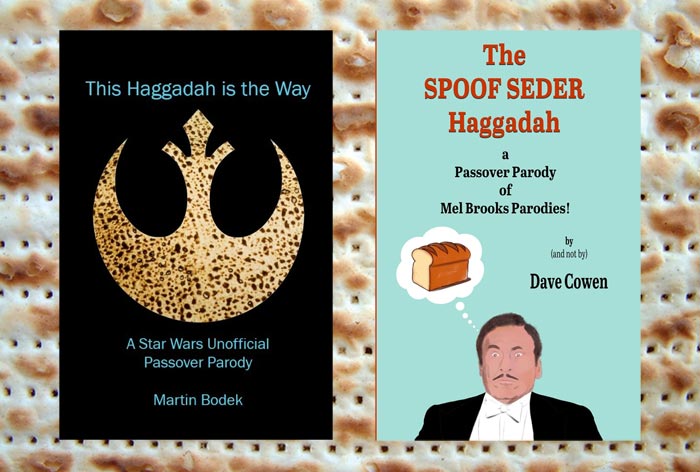
Fun Haggadot for Passover

UC Berkeley Law School Dean Talks About Antisemitism on Campus
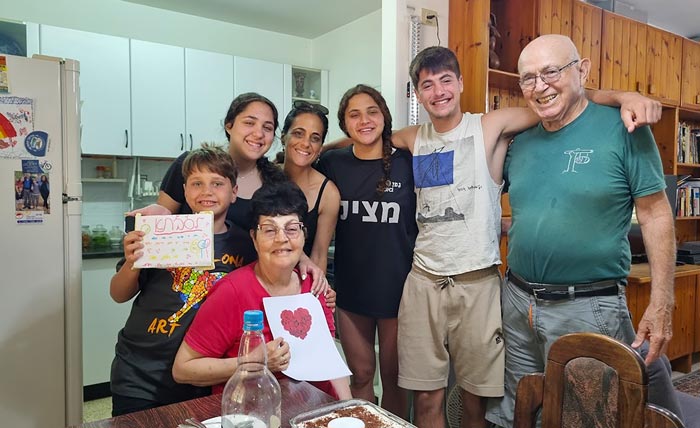
Father’s Captivity in Gaza Spurs Family’s Tireless Advocacy for Hostage Release

Understanding the As-a-Jew Jew

 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.