
Category
cancer


JScreen Is Making Cancer Genetic Testing Accessible
Ari Noonan
May 13, 2021
Ashkenazi men and women face a 1-in-40 risk of carrying mutations in the BRCA1 and BRCA2 genes (genes linked to breast, ovarian, prostate, pancreatic and melanoma cancers) — more than 10 times the risk in the general population.


Jewish Organization Sharsheret Helps Women with Breast and Ovarian Cancer During Pandemic
Erin Ben-Moche
October 23, 2020

My Mother’s Warfare Against Aesthetics
Rebecca Katz
October 12, 2020
My mother was a fierce, stubborn, hard-working woman. She was also a woman who cared about her appearance and deeply internalized the aesthetic pressures on women.

Jewish Community Mourns the Passing of Rabbi RBO Bat-Or
Jewish Journal Staff
October 2, 2020
Rabbi RBO leaves a legacy any of us would be lucky to achieve — one marked by a deep drive to make the world a more just and equitable place.

Jason Alexander to Emcee Virtual Israel Cancer Research Fund Gala
Erin Ben-Moche
July 15, 2020
Tom Brokaw, Aaron Ciechanover, Eugene Levy and Benj Pasek, join in the star-studded evening supporting Israel cancer research.



New Articles

LA Congresswoman Sydney Kamlager-Dove Votes Against Resolution Declaring “From the River to the Sea” Is Antisemitic
Kylie Ora Lobell
April 17, 2024

ADL: Antisemitic Incidents Increased 140% Last Year
Aaron Bandler
April 17, 2024
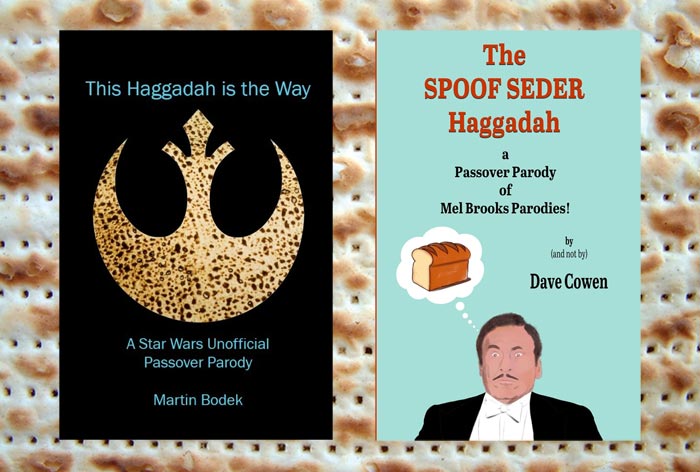
Fun Haggadot for Passover
Debra L. Eckerling
April 17, 2024

UC Berkeley Law School Dean Talks About Antisemitism on Campus
Alan Zeitlin
April 17, 2024
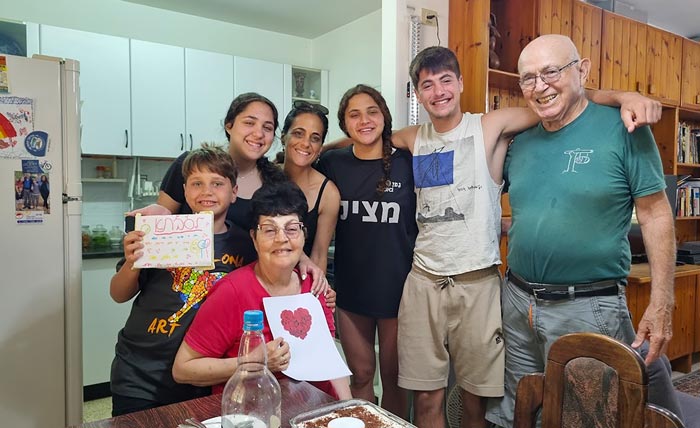
Father’s Captivity in Gaza Spurs Family’s Tireless Advocacy for Hostage Release
Ayala Or-El
April 17, 2024
 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.