
Category
alzheimer’s

When Harry met Lilly…
Rabbi Harry Roth will read this article aloud to his wife, Lillian, after it’s published.
With electromagnetics and metal caps, Israeli companies aim to zap brain diseases
It looks like a futuristic salon hair dryer. Connected to a computer by a bright orange strip, the half-cube with rounded corners sits comfortably atop the head, a coil of wires resting on the skull.
USC seeks twins with Alzheimer’s for study
Researchers at the University of Southern California are seeking twins with Alzheimer\’s for a study that seeks to help researchers understand risk factors for the disease. Participants will be interviewed about their life histories and their experience with Alzheimer\’s. The interviews can take place by phone, in the homes of the participants or at the university campus.
Getting to know my dad, again
My 93-year-old father emerged as a different person when my mother was diagnosed with Alzheimer’s five years ago. He became independent, assertive, interested and engaging. When my mother died in October, he even became a bit spiritual. He’s certainly not the exhausted father with whom I grew up, who often didn’t know what to say to me. As a teenager and young adult, I never thought we would have much of a relationship. But now, as I approach 60 and he nears 94, the engagement between us has blossomed, as it has with my brother and all our children. The relationship he now has with my wife has become his most significant. She handles his money.
Pingpong therapy brings net gains to Alzheimer’s patients
Usually, Fryda Dvorak needs a cane to move around. But put her behind a pingpong table and you wouldn’t know it. Dvorak, 86 and living with early-stage Alzheimer’s disease, returns volley after volley with her confident lob, sometimes gritting her teeth in concentration as she reaches to hit the ball. She’s so focused on the game that she refuses to put the paddle down for a breather when her instructor, Irina, suggests they take a break.
Searching for the soul
In my new capacity as the son of an Alzheimer\’s victim, I have many questions. Some of them are Jewish questions. One kept me up for hours the other night, leading me to my bookshelf at 3 a.m., combing through volumes to see what insights I might glean. What happens to the soul during Alzheimer\’s?
The emotional landmines of family caregiving
A painful situation for the primary caregiver occurs when another close relative does little or nothing to help, but they are adored and praised by the senior anyway.
Films: Dementia ordeal inspires comic tale of ‘The Savages’
Tamara Jenkins knows firsthand what an overwhelming task it is to care for a parent suffering from dementia. While she was in her mid-30s, she had to help care for both her father and grandmother during their final days in a nursing home. She also knows that no matter how grave a situation might be, there are always sparks of humor surrounding it. So it\’s no surprise that her new film, \”The Savages,\” addresses that very subject and does so with a healthy dose of comic perspective.
New Articles

Print Issue: Mr. Hasbara | April 26, 2024

BRAVE-ish on ReachTV Where Next!

On Counting the Omer
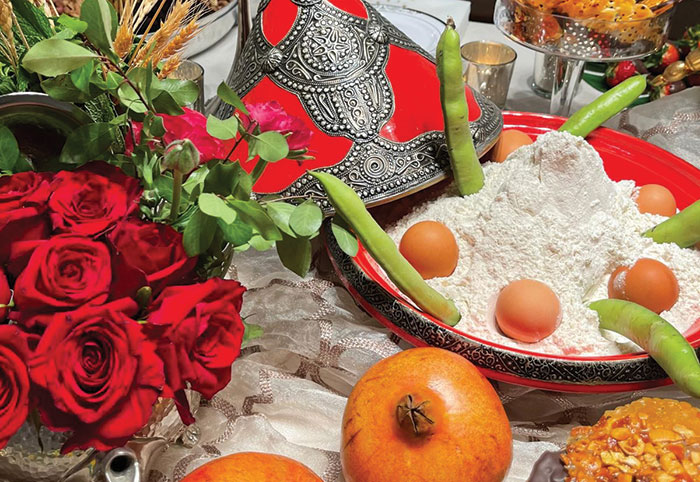
A Memorable Mimouna

 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.