If a terminally ill patient requesting a prescription for aid-in-dying medication approaches Dr. Gary Schiller, a Reform Jew and hematologist with the UCLA Health System, Schiller already knows what he’ll answer.
“I will certainly not practice according to this law,” he said, referring to the California End of Life Options Act, which as of June 9 permits physician-assisted death under certain conditions.
Instead, Schiller would ask the patient some questions: Where does his or her desire to die come from? Would the patient be more comfortable with palliative treatment or hospice services? Does he or she want to withdraw from medical care?
“It will come up,” he explained. “Sometimes you give people narcotics to the point where you might hasten their death in the intent to control pain. But intent is everything. The intent to alleviate suffering is not equal to the intent to deliver death.”
California’s new legislation, like that of four other states, affirms the right of terminally ill adults diagnosed to live only six months or fewer to request, receive and self-ingest lethal medication. The patient must have full decision-making capacity and be deemed medically competent by two physicians. However, the law does not require health care providers, including physicians, nurses and entire facilities, to participate in the aid-in-dying process.
Support for this law grew after the highly publicized death of 29-year-old Brittany Maynard, who moved from California to Oregon in 2014 after being diagnosed with brain cancer so she could take advantage of Oregon’s aid-in-dying legislation. According to a February 2016 report by the Oregon Public Health Division, 991 Oregonians have died from intentionally ingesting prescribed lethal medication since the passage of state’s 1997 Death with Dignity Act.
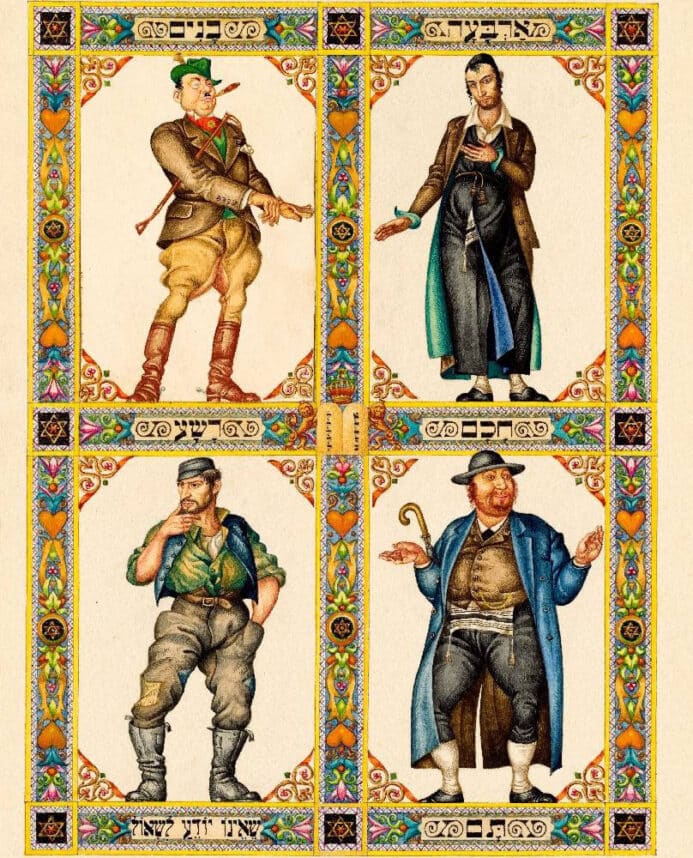
Rabbis interviewed across Jewish movements agreed on the principle of pikuach nefesh, the preservation of human life, as the main reason to oppose physician-assisted death. While the majority maintained that physician-assisted death is halachically prohibited, a few identified extraordinary exceptions when taking into account other Jewish values.
Rabbi Dr. J. David Bleich, a Talmud professor at Yeshiva University’s Rabbi Isaac Elchanan Theological Seminary, who has written extensively on Jewish bioethics, said that physician-assisted death is “a topic of which there is relatively little to say.”
“Suicide is not permissible nor is assisting in suicide permissible,” he said. “Absolutely no exceptions. The [terminally ill] patient should be kept from pain.”
Moreover, Modern Orthodox Rabbi Jason Weiner, who leads the chaplaincy team at Cedars-Sinai Medical Center, explained it is possible to differentiate between physician-assisted death and a case where a terminally ill patient decides to stop taking medication.
“Jewish Law sometimes sees passive inaction (shev v’al taaseh) as being less prohibited than actively doing something, so there could be cases in which it would be permissible for a dying patient to forgo certain aggressive interventions or medications, with the approval of an experienced rabbi,” he said.
In agreement, Morateinu Alissa Thomas-Newborn, a clergy member at the Modern Orthodox congregation B’nai David-Judea, indicated that physician-assisted death is halachically prohibited and could be compared to murder.
“[T]he value of life, and more importantly, the value of God’s role in the giving and taking of life are tantamount in this prohibition,” she wrote in an email.
But Thomas-Newborn explained that there still exists a religious obligation to alleviate suffering for those at the end of their lives. She cited Rabbeinu Nissim, who allowed people as a means of attaining comfort to pray for the death of someone suffering from a terminal illness (Ran on Nedarim 40a), as well as Rabbi Moshe Feinstein’s approval for the withholding of medical interventions that only extend the pain of a terminal patient (Responsa Iggrot Moshe, Yoreh Deah, 174:3).
Rabbi Elliot Dorff, chairman of the Rabbinical Assembly’s Committee on Jewish Law and Standards, wrote a rabbinic ruling for the Conservative Movement in 1997 on assisted suicide. He says the law could be applied only in “very rare” cases where uncontrollable pain is the sole motivator behind a person’s request to die.
“Saving a life is the most important obligation except for three things — murder, adultery/incest and idolatry,” he said (Sanhedrin 74A). “Even during the Holocaust, you had these excruciating circumstances when people could have committed suicide but didn’t.”
“You get, in the tradition, a clear rule that you cannot hasten a person’s dying process or delay it, either,” Dorff said (Yoreh De’ah 339:1). In his ruling, he cited the talmudic story of Rabbi Hananyah ben Teradyion, who refused to expedite his own death by opening his mouth to breathe in fumes from flames when he was set on fire by the Romans.
Dorff also expressed concern for coercive pressures a terminally ill patient may face.
“Anytime you deal with assisted suicide, all kinds of factors come into play — a dad wants to leave money to his children, or children don’t want their dad to squander family money,” he said. “Part of the problem with assisted suicide is that often it’s not because there’s a medical reason, it’s because people don’t think anyone cares if they live or die.”
Rabbi David Teutsch, director for the Center for Jewish Ethics at the Reconstructionist Rabbinical College, said he doesn’t consider himself “explicitly bound” by halachah when addressing this issue.
“If a person is fatally ill or in a lot of unmanageable pain, that would be a justification in my mind to seek out a medicine to alleviate the pain or indignity,” he said. “The unconstrained notion of saving a life trumping all other concerns was developed at a time when medicine was extremely primitive. They certainly could not have looked ahead to life-preserving measures we find in any major hospital.”
To develop a policy with regard to the new law, Los Angeles Jewish Home, the largest Jewish senior living organization in California, has established a task force chaired by Dorff.
“Our main focus for that committee is to assure that whatever our policy is, it’s connected to our mission — which includes care related to Jewish values,” said Dr. Noachim Marco, chief medical officer of Los Angeles Jewish Home.
Notably, Cedar Sinai Park, the only Jewish senior-care home in Portland, Ore., does not have a policy regarding whether patients may take aid-in-dying medication on its premises, said CEO Sandra Simon. However, if residents choose to take a lethal dose, staff members may not participate.
Rabbi Carla Howard, a conservative rabbi who directs the Jewish Healing Center of Los Angeles, said the new law is “short-circuiting hospice.”
“Spiritual care is about showing up and being there for the person should they want to wrestle with this,” she said. “Some people are uncomfortable with the notion that they don’t get to run the show. Unfortunately, life is about that process and not knowing.”
Dr. Neil Wenger, who is Jewish and the director of the UCLA Health Ethics Center, said that at least initially, patients will not be permitted to take the drug inside UCLA hospitals in order to respect the views of staff members who disagree with the law.
“There is absolutely no pressure for that physician to prescribe medication,” he said. “We will help to facilitate finding other physicians who might be willing to prescribe under the circumstances.”
Even if UCLA hospitals never prescribe the medicine, Wenger thinks the discussion the law has sparked is imperative:
“[We need] to ask: Why is this patient [requesting] this medicine? Could I have found a support group for them? Referred them to a social worker? What is it that I could have done so they wouldn’t feel the need to request this medication?”



















 More news and opinions than at a Shabbat dinner, right in your inbox.
More news and opinions than at a Shabbat dinner, right in your inbox.